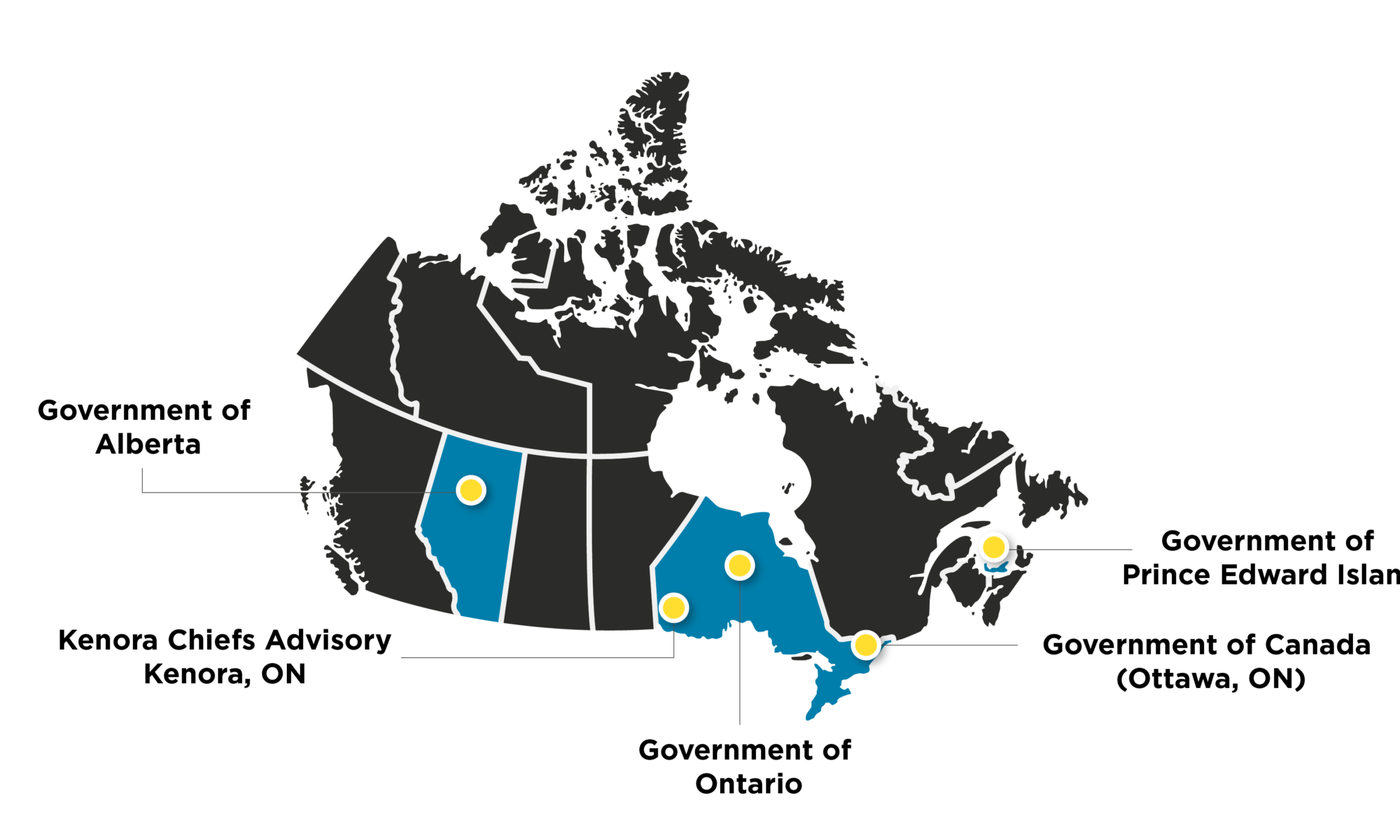
No More Islands of Care: Bolstering mental health and addictions services for pandemic & post-pandemic life on Prince Edward Island
Series | Public Service Innovation and Leadership During COVID-19Prior to COVID-19, Prince Edward Island struggled to keep up with demand for mental health and addictions services. Now, after pivoting to virtual care in response to COVID, P.E.I. has more psychiatrists on-call and more options for support. Good thing, because the long-term stresses brought by the pandemic have made mental health and addictions services more critical than ever before.
Despite being a psychiatrist, Dr. Heather Keizer speaks with the urgency of an emergency room doctor treating a trauma patient. That’s on a normal day. It’s no surprise, then, that in mid-March, as some hospitals across the globe became overrun with COVID-19 patients, Keizer expected her team to take on the same rapid-fire energy in preparing for an outbreak.
“We had to act very quickly,” said Keizer of her team and colleagues at Health PEI. “We thought we had New York on our hands – or Italy.”
Anticipating the Island could get hit with a storm of COVID infections, Health PEI’s top priority was to free up hospital beds, and to encourage Islanders to stay home.
This meant Keizer, as the province’s Chief Medical Officer of Mental Health and Addiction, had to mobilize her team to discharge psychiatric patients from hospitals, come up with a means to continue treating severely ill psychiatric patients safely, and, ultimately, adapt services to support an island of people increasingly vulnerable to addictions and mental health challenges.
“It was a herculean effort,” Keizer would say on CBC Television in March – only two weeks after the World Health Organization declared COVID-19 a global pandemic. She went on to say that in such a short timeframe, their department had proven to be “more nimble” than before.
Within little more than a month, P.E.I.’s Mental Health and Addiction team was able to shift service delivery sites, introduce virtual care, hire more psychiatrists, significantly reduce wait times for psychiatric assessments, and expand its service options.
“We were having to change literally everything we did over COVID,” said Lisa Thibeau, Administrator for Addictions Services East.
P.E.I. had, for a long time, struggled to keep up with demand for psychiatric care. Now, it finds itself closer to its long-term strategic goals for service delivery, and more equipped to handle future medical crises, as well as, quite possibly, upcoming mental health crises.
Clarity and an “Intimate Command Centre”
Keizer believes the speed with which MHA was able to pivot its operations was due, in part, to “physician leadership” – the ability to make quick decisions in an emergency “because that’s what we’re trained to do as physicians.”
It was also due to a “singular focus on the pandemic,” said Verna Ryan, the department’s Chief Administrative Officer. And, she said, the MHA leadership’s emphasis on communication.
Their teams suddenly had no other priorities than to respond to COVID. Schedules were freed up. Calendars wiped clean. Important work put on hold. They were able to “stop the factory belt” and re-focus on COVID: how to keep people safe; and maintain, if not grow, services under the new constraints of social distancing.
Ryan and Keizer called regular meetings, immediately. Staff would get on a conference call together no fewer than three times a week in March and into April. There’d be up to 40 people on the larger lines. Breakout calls were held for smaller teams.
Communication would go up and down the chain – from a Joint Response Committee – to all team members, with everyone looped in. They’d share big-picture items – updates from Canada’s Chief Public Health Officer, to personal concerns.
“These calls became what we were living and breathing,” said Ryan. “We became an intimate command centre.”
But unlike many pre-pandemic meetings, the command centre’s were laser-focused.
The mandate: ensure hospitals had enough beds to accommodate potential COVID patients, while preventing exposure to the virus for as many people as possible. Keizer decided this would require moving up to 72 patients from the psychiatric ward at Hillsborough Hospital — creating discharge plans and community supports for those determined safe to leave, and relocating others to Prince County Hospital — all within a few days. Then, they would have to find another way to provide urgent psychiatric care, and make mental health and addictions services available across the island, virtually.
“We had very clear direction,” said Joanne Donahoe, Director of Program Planning and Coordination. “The options weren’t, ‘Could we do this?’… It was, ‘This is happening’.”
The question became, How? How to protect patients and staff? How to abide by World Health Organization guidelines? How to re-deploy staff? How to communicate changes to the public? Process mapping, IT support…
Every situation was “like a Sudoku puzzle,” said Ryan. But this time, it was unconstrained by the usual systems and processes. Bureaucratic barriers that would normally have delayed or stopped initiatives, fell away.
“It really was a unified front,” said Ryan. “We had a unified ‘enemy,’ if you will, in COVID.”
Their unified response catalyzed major changes to the province’s psychiatric services, including dramatically reducing wait times for psychiatric care.
Introducing Psychiatric Urgent Care Clinics
In recent years, if someone in P.E.I. were experiencing an acute mental health issue – perhaps suicidal ideation, extreme panic or severe depression – they would go to a hospital emergency unit and find themselves waiting, on average, 18 hours to be discharged or admitted.
“Sometimes they would feel as though they weren’t sure if anyone was going to come,” said Lorna Hutt, a community manager for MHA west. “They’d sit and they wouldn’t have a sense as to where they were.”
Now, people presenting for psychiatric care are seen within an hour.
In fact, by April 1, mere weeks after the province declared an emergency, the MHA team had found a way to see people with acute needs almost instantly. They developed Psychiatric Urgent Care Clinics with virtual, on-call psychiatry – what Hutt calls a “totally fantastic, enhanced service.”
The idea for the clinics came about serendipitously. While everyone at MHA had shared a desire to speed up service times, their first goal in March was to prevent people with mental health and addiction issues from exposure to COVID.
They’d already shuffled dozens of psychiatric patients to make space for potential COVID cases; now they needed to get creative about providing those people, and others who might soon present to hospitals, with urgent care.
One of their acute care leads, Leslie Warren, had the idea to divert patients away from hospital emergency rooms by creating a temporary set-up in an unused space at Hillsborough. This set-up became known as a Psychiatric Urgent Care Clinic, or “puck.” A second PUCC opened two weeks later in Summerside.
At the new clinics, people can present without an appointment, just like in the ER. A crisis nurse or social worker greets them within an hour and sets them up with a virtual, on-call psychiatrist. This doctor assesses them remotely via Telemerge, a video conferencing system, and determines their needs – whether to be admitted, connected to detox services, connected to Social Development Housing if they don’t have a secure place to stay, or provided with a safety plan to go back into the community.
“I had a vision in my head about this before COVID started,” said Keizer. “I wanted to have (virtual health care) within our walk-in clinics. But it’s a novel idea for a lot of people. And I think COVID gave us a catalyst to be able to do it, when previous efforts to do it were, perhaps, a little more challenged by the system – I’ll put it that way.”
In this case, Information Technology support staff, corporate services, psychiatric and social work services collaborated to create a process map and prepare procedures and protocols for every part of the patient experience.
They designed a program “from scratch to implementation,” something Donahoe says would normally be impossible to do in even 18 months.
“Here we had weeks,” she said. “We were told to do it. Get it done. The costs? We would capture them, record them. But (we were told), ‘you’ll figure that out later’.”
Virtual psychiatric services didn’t only expedite the assessment of acute care patients, it also allowed for round-the-clock availability without the usual geographic and staffing constraints. And it meant doctors and patients could reduce their risk of exposure to COVID.
The province provided laptops and iPads to nursing homes and acute care residences so psychiatrists could see clients who were distressed or having behavioural problems.
Normally, Keizer’s team would also have been limited by a small roster of available psychiatrists – not enough to provide care on evenings and weekends. But the PUCC service model included a new 24-hour follow-up practice to prevent staff from losing track of patients with acute needs who may be prone to harm or relapse. So Keizer applied under COVID support funding to hire more administrators and psychiatrists from out of province – so long as they attained a licence to practise in P.E.I.
Before COVID, the province faced a backlog of nearly 1,200 people awaiting psychiatric assessments. The wait time for an adult to see a psychiatrist was often more than a year, according to Keizer. “And in the ballpark of 150 to 200 days to see a child and adolescent psychiatrist.”
With the COVID-inspired staffing boost and virtual accessibility, Keizer says her team had cut the adult waitlist down 60% by July, and 100% for children and adolescents.
‘I had a vision in my head about this before COVID started. I wanted to have (virtual health care) within our walk-in clinics. But it’s a novel idea for a lot of people. And I think COVID gave us a catalyst to be able to do it when previous efforts to do it were, perhaps, a little more challenged by the system.’ – Dr. Heather Keizer, Chief Health Officer, Mental Health and Addictions, PEI
Island-wide virtual care
Surprisingly far fewer people initially presented to the PUCCs or mental health centres in the early weeks of COVID than anticipated. People seemed to hunker down at home, whether following WHO guidelines or out of anxiety over contracting the virus.
“There was such a fear-factor related to COVID,” said Ryan about people’s treatment-seeking behaviours. “I don’t think that that can be underestimated.”
When people did present in April and onward, they were sicker, she said. Their conditions had worsened. Some turned to substances to cope. Demand for detox went up, as did the risk of domestic violence.
The need to provide virtual care across the island was obvious immediately. Clinicians working from home could only get so far by phone. They needed eyes-on to provide proper consultations. And support group members needed the opportunity to make eye contact with counsellors and their peers.
Keizer and Ryan lobbied for a video conferencing platform from the get-go.
Kim Knox, Dr. Greg German and Ryan Hennessey formed a project team assigned to procure and deploy a software system across the province – Knox, as the business lead, German as medical, and Hennessey as the head of tech.
Knox sat on a jurisdictional committee of Canada Health Infoway, a federally funded non-profit tasked with accelerating the adoption of digital health solutions. That’s where Zoom for Healthcare came on her team’s radar. It was a top contender for virtual services among provincial health care providers.
The trio put together an expedited procurement process to evaluate a couple of different tools – a process that would normally take six months, according to Hennessey, was reduced down to one month. “We had to be a little more fluid with our requirements,” he said.
They landed on Zoom for Healthcare, then had to convince the province it was a specialized product, not the kind strangers could hack and infiltrate, or “Zoom-bomb.”
“We had to get everyone settled that we weren’t using the same Zoom that was being exploded out in a lot of the news at the time,” said Hennessey. “I think that made a lot of people nervous.”
Zoom’s industry-specific Zoom for Healthcare, they determined, followed Canadian and U.S. privacy acts. It differs from Zoom’s more popular chat products, Hennessey said, in that it has hundreds of specifications they could disable and lock down as security measures.
Once the province approved their selection, they formed another team to develop workflows and training webinars. Then, had to deploy Zoom for Healthcare to all of the clinicians across the island, provide laptops, headsets and cameras, get clinicians licenced and hope for as little learning-curve as possible.
Among clients, there was a “continuum of reactions”, said Hutt. “We had folks who struggled with attending virtually and would forget or didn’t like it. They weren’t comfortable with the technology side and felt it just wasn’t the same as meeting in person. … And then we had those right on the other end of the spectrum who loved it and feel like they can get a quicker check-in session over Zoom … it was a comfort and welcome that they were able to get that support in home. So the whole gamut.”
More people are now signed up for those support and therapy groups that MHA now deliver virtually than there had been for in-person sessions before COVID.
P.E.I. has about 160,000 residents, 40,000 of whom are concentrated in Charlottetown, the capital. The rest are spread across nearly 6,000 square kilometres. It could take up to two hours to drive to the city centre from the furthest point.
Offering virtual health care provides rural residents with greater flexibility to attend appointments. Clients who may find it hard to drive into Charlottetown, or would have to juggle childcare and other costs, can now get help from home.
“I think it’s a good use of everyone’s time,” said Donahoe. “It’s a very value-added service that we’d love to see continue.”
“Not out of the woods yet”
COVID-19 did not hit the Island the way many had feared.
The province had its first case on March 14. Two days later, Premier Dennis King announced a provincial state of emergency. The Island quickly shut down its borders and restricted non-essential travel. Most schools and businesses closed.
By mid-October, fewer than 60 people had contracted the virus. No one died.
The province was lauded for its success in containing COVID’s spread. But while social distancing practices have kept the virus at bay, Health PEI’s Mental Health and Addiction department faces a growing threat. The global pandemic continues. And the more that people are locked down, and the longer they face uncertainty about their futures, the higher their chance of experiencing mental illness.
“None of us is escaping the effects of this,” said Dr. Jacqueline Roche, on a local radio station in April. “It’s an impossibly hard time. And the most important thing I think we can do is just make space for that.”
Roche is a clinical psychologist for children and youth, and heads the children’s unit in P.E.I.’s central region. She spoke on Ocean 100 as part of MHA’s way to not only promote their new virtual services, but also to help parents reframe their stress, learn ways to cope, and support their families.
In the early stages of COVID response, her team’s approach shifted somewhat from an exclusive focus on service delivery and helping people get better, to preventing them from getting worse.
“I mean, our hope at that point was really to maintain people,” said Roche. “Supporting people to stay well, or to stay – to kind of plateau, right?”
Her team worried financial impacts, the stress of unpredictability, and limited social interactions would exacerbate an already challenging situation.
In April, P.E.I. had the highest unemployment rates in the country. The Island relies on tourism, but with borders closed, their second-largest industry took a drastic hit.
Employment rates have generally been improving since then, assisted in part by relaxed travel restrictions between the four Atlantic provinces (the “Atlantic bubble”) beginning in July.
Still, by the end of the summer, about half of all national respondents surveyed by the Canadian Mental Health Association reported feeling anxious or worried.
“Across the country, 38% of people said their mental health had declined due to COVID,” said Tayte Willows of CMHA, speaking to P.E.I.’s Legislative Assembly on Sept. 30.
Willows reported a 140% rise in suicidal thoughts.
Roche’s greatest concern is for youth, who she says account for 75-80% of those who present to emergency rooms in suicidal crises.
So, just as MHA had developed a new 24-hour follow-up practice at their PUCCs, Roche’s community team – and her peers across the Island – developed Child and Youth Mental Health Clinics in response to COVID-19. Units that would offer 24-hour response times for young people seeking urgent care.
A child or youth who now calls a mental health line will be connected to treatment within no more than a day, said Roche, even if their call comes on a weekend.
“It’s a real caring, safety-net model for suicide,” said Roche. The approach has allowed community teams to support young people in crises outside of an emergency room and inpatient model.
And it allowed MHA to dramatically reduce the need for hospitalization – their initial goal in the face of a pandemic.
But while hospitalization rates of COVID cases remain low, mental health and addictions concerns are on the rise.
Roche points to Maslow’s Hierarchy of Needs. The psychology theory shows that in order for humans to survive they must first have their physiological needs met: food, warmth, clean air. Then, they need safety, social connection, love, belonging and a sense of self-worth. Staying cooped up can prevent contracting a virus, but still poses a challenge to survival, especially in the long term.
Speaking on the radio, Roche wanted parents to accept that all feelings – grief, fear, uncertainty, anger – are valid, both for adults and children.
And she wanted people to seek connection, to collectively manage their fear.
“This is hard. This is hard stuff. Nobody’s prepared for this and nobody signed up for this,” she said. “It’s about being brave and vulnerable and asking for help. There’s no shame in that. We’re all going through this together. And I think we’ve got to stick together if we’re going to get through it.”
The Island is “not out of the woods yet,” in Keizer’s words. COVID remains a rapidly changing situation.
Roche worries that this winter may be harder than at the outbreak of the pandemic, because of the chronic exposure to stress which can cause more acute conditions.
But today, P.E.I. is better equipped to respond to hospital intake needs, and to provide socially distanced care, than before COVID. Mental health and addiction services are now accessible anywhere that has a strong Wi-Fi signal.
The Island went from struggling to keep up with demand for psychiatric care in the years leading up to 2020, to now employing more psychiatrists than ever before.
The team at MHA has proven it can achieve “herculean” feats that fast-track and enhance service standards when members pool their strengths, focus on a clear vision, communicate updates, think creatively and work within relaxed systems.
It’s also proven, more widely, that mental health and addictions services play a critical role in a population’s overall health. And, that MHA is a provincial department that can lead in decision-making and innovation.
“Early on I think the perception was that (MHA) really wasn’t a problem because we’re not medical, right?” said Keizer. “We’re not dealing with COVID. It’s not medical.”
But her team’s response to COVID has proven they do valuable and ground-breaking work.
“That was a big learning point,” said Keizer. “Just because we’re mental health and addictions, just because we’re second, doesn’t mean we can’t lead the charge in terms of being innovative. That’s important.”
The Government of Canada, The Wilson Foundation, The Lawson Foundation and Microsoft.