Report 5: Reaching the Vaccine Hesitant
Series | COVID-19 Vaccine Skepticism in CanadaIntroduction
To date, more than 17 million Canadians have been vaccinated, including more than 1.1 million who have received two doses. There is, however, still a long way to go. First shots need to be administered to more than 10 million Canadians, and more than 25 million second shots will need to be administered. Meanwhile, physical distancing and other preventive measures need to be maintained. As importantly, those who have not yet been vaccinated—because of hesitancy, not vaccine unavailability— need to be convinced to roll up their sleeves.
Until now, supply and delivery capacity have limited the rate of vaccine roll-out. But this will soon change. Within months, if not weeks, the limiting factor on vaccination rates will be the willingness of otherwise–reluctant individuals to be vaccinated.
The purpose of this report is to provide a real–time view of the vaccine hesitant. There is no shortage of research on who is and is not willing to be vaccinated but this research has limited applicability to the COVID-19 vaccine roll-out for two reasons. First, much of it concerns childhood vaccinations, and the choices parents make on behalf of their children, which is not applicable to the roll-out of COVID-19 vaccines at present. Second, like pandemics, en masse vaccine rollouts are rare. Accordingly, taking an in-the-moment view of who is vaccine hesitant and what factors structure their hesitancy can help us better understand how to confront the challenge of the last stages of mass vaccination.
In what follows, I present data demonstrating that vaccine willingness has increased in Canada in the last four months—impressively so. Still, some 20% of Canadians remain reluctant. Tackling vaccine hesitancy requires that we understand their views. Who are these people? Where do they live? How informed are they about COVID-19? The answers to these questions lead to recommendations about how Canada can speed up vaccine uptake.
Data
This report relies on data collected through the Media Ecosystem Observatory (MEO), a collaborative effort of three research sites—the Centre for Democracy, Society, and Technology, the Social Dynamics Lab at McGill University, and PEARL at the University of Toronto. MEO was born out of the Digital Democracy Project, of which the Public Policy Forum was an early funder and champion. Since the third week of March 2020, MEO has conducted more than 92,000 interviews of Canadians in over 45 waves of data collection, all focused on the social and political contexts and implications of the COVID-19 pandemic. A longer description of our research strategy is available at mediaecosystemobservatory.com.
The data presented here were collected from the 30th to the 45th wave, from Jan. 18, 2021 to May 11, 2021. The total number of effective respondents is 24,629. Respondents were recruited by Dynata to complete a survey hosted on the Qualtrics platform. Iterative proportionally fitted weights are generated using levels from the Canadian census and are applied to our data within each wave.
Results
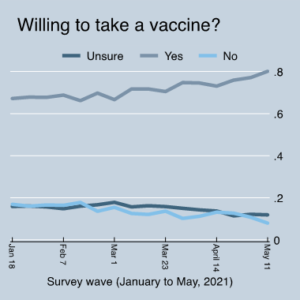
Figure 1: Changes in vaccine willingness over time
Figure 1 demonstrates willingness to take a vaccine since January 2021. (MEO has been collecting data on this question since June 2020.) Importantly, this is the beginning of the period in which Health Canada approved vaccines for use. These vaccines had started their roll-out across Canada, although initial distribution was targeted to the elderly living in long-term care homes and those working on the front lines of health care. Importantly, this is also the period in which some other countries—notably the United States and the United Kingdom—got a major jump on vaccinating large parts of their populations. In short, this was when the choice to be vaccinated became real.
In this period, vaccine willingness has increased markedly. By the middle of January—the start of the time series in Figure 1—67% of Canadians were willing to take a vaccine or already vaccinated. The shares that were unsure or unwilling were largely equal, at 16% and 17% respectively. Importantly, these numbers were stable since MEO began collecting data on vaccine willingness, in June 2020. Since January 2021, however, vaccine willingness has increased, reaching 80% by May 11, 2021. Where has this 13-percentage-point increase come from? In the aggregate, it has been generated by a decrease of nine percentage points of Canadians saying no to vaccines, and a decrease of four percentage points in those saying they are unsure.
It is clear that vaccine hesitancy is decreasing. But among those who remain vaccine hesitant, what factors explain this reluctance? Our data allow us to identify three broad sets of factors.
The first are well-known demographic factors. Namely, we explore whether vaccine willingness is correlated with education, income, age and gender. We also explore whether vaccine willingness is correlated with being racialized. The goal here is to understand which largely fixed factors may be structuring vaccine willingness.
Second, we consider geographic factors. In particular, we look at the effect of living in rural versus suburban or urban locations, and, in an analysis limited to the Ontario data, whether people living in a “hot spot”—as defined by the broad geographic catchall of the first three digits of a postal code or “forward sortation area”—are more or less likely to be willing to be vaccinated.
Third, we explore numerous attitudinal and behavioural factors which previous modelling suggests matter for COVID-19 opinions and behaviours generally and vaccine willingness specifically. These factors include how concerned individuals are about the risk of COVID-19 to themselves and others; how much they follow news related to COVID-19; how misinformed they are about COVID-19; and how mistrusting they are of experts, which we call anti-intellectualism. For a longer description of these factors, please see related work with Eric Merkley on anti-intellectualism.[1]
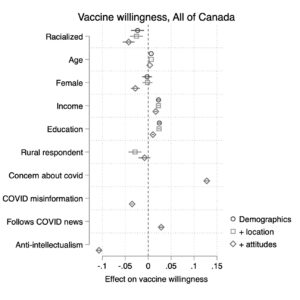
Figure 2: Vaccine willingness among all Canadian respondents. Results are from OLS models of vaccine willingness, modelled on demographics with stepwise addition of location and attitude variables. N=24,629
Figure 2 presents results from regression models of vaccine willingness, modelled on all Canadian respondents from January 2020 to May 2021 (N=24,629). We estimate three models: one with only demographics, another adding geographic information and a third adding attitudinal and behavioural measures.[2] Several important insights emerge.
First, looking at demographic factors, we see that age is weakly correlated with being willing to be vaccinated, while being female is negatively correlated, particularly after taking account of non-demographic factors. Those people who have a higher income and/or more education are more willing to be vaccinated. Finally, net these other factors, we find that racialized people indicate a statistically significant lower willingness to be vaccinated. The effect is not substantively overwhelming, but it is real.
When examining the geographic factor of living in a rural area, it too is negatively correlated with being willing to be vaccinated. That said, the effect of living in a rural place is measurably reduced once accounting for attitudinal differences between individuals. Turning to behavioural and attitudinal measures, concern about COVID-19 has an outsized effect on willingness to be vaccinated—indeed, it is greater than any other single factor. Trust in experts and scientific expertise is also strongly related to vaccine willingness; those who are higher in anti-intellectualism are markedly less likely to be willing to be vaccinated. Finally, though comparatively smaller in effect, reading news about COVID-19 is positively associated with willingness, while being misinformed is negatively associated with willingness.
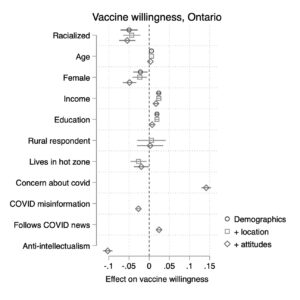
Figure 3: Vaccine willingness among all Ontario respondents. Results are from OLS models of vaccine willingness, modelled on demographics with stepwise addition of location and attitude variables. N=9531.
Figure 3 presents results when we limit the analysis to Ontario (N=9,531), which allows us to incorporate an indicator of whether an individual lives in a “hot spot.” The results in this model are largely consistent with those presented in Figure 2. Accordingly, I do not present them exhaustively here. Zeroing in on hot spots, those who live in hot spots express a lower willingness to be vaccinated, net all other factors.
Recomendations
We are on the last two miles of the journey of vaccination.
In short order, the majority of Canadians will have received a first shot. The two big remaining tasks are to encourage people to seek second shots, and to convince those who are still hesitant to be vaccinated.
While encouraging second shots is not the focus of this report, it is worth noting that Canada’s fundamental lack of centralized, systematic health care data is a barrier to coordinating second doses, especially with rapidly changing supplies and usage guidelines. Governments will likely rely heavily on the data infrastructure of private providers (i.e., pharmacies) and semi-autonomous public bodies (i.e., regional health authorities). No doubt, many citizens will also be asked to spend hours hunting for their second shots. None of this is acceptable and it should be addressed before the next pandemic.
How can the vaccine hesitant be persuaded, in the meantime? Based on the findings of this report, three recommendations can be made.
1. Public health communicators must communicate the continued threat of COVID-19.
Convincing the vaccine hesitant to roll up their sleeves may become more, not less, difficult as time goes on. Concern about vaccine side effects will hopefully subside as mass vaccination demonstrates the safety of approved vaccines. However, mass vaccination will reduce the overall threat of COVID-19, which should in turn reduce citizens’ concerns about the disease. Given that concern about COVID-19 is the single biggest predictor of willingness to be vaccinated, any decline in concern will increase vaccine hesitance. Public health communicators must be creative and focused in communicating the continued threat of COVID-19—including the possibility of a fourth wave—if we are not able to reach sufficiently high levels of vaccination.
2. Federal and provincial governments need to ensure clear and consistent vaccine messaging.
A lack of trust in scientific expertise—what we call anti-intellectualism—is a major predictor of vaccine hesitancy. This mistrust is perpetuated by continued mixed messages around vaccines. In as short an order as possible, federal and provincial governments need to determine a method to ensure clear and consistent messaging on vaccines. Science must be at core of decision making around vaccines, but it need not be worked out in real time in front of the cameras.
3. People and communities who are most likely to express vaccine hesitancy should be reached to reduce hesitancy, and the search and transaction costs for being vaccinated should be reduced.
Vaccine hesitancy is slightly higher among those with lower levels of education and income, those who live in hot zones and those who are racialized. None of these differences are impressively large, but their cumulative effects matter for public health outcomes. Public efforts to address vaccine hesitancy should target those individuals and communities who are most likely to express vaccine hesitancy, while recognizing and respecting the basis of such hesitancy. It is also important to recognize that these factors are often stand-ins not only for differences in beliefs, but also differences in resources. Being vaccinated takes time, especially when finding a vaccination site takes searching. Decision makers must do everything possible to reduce the search and transaction costs for obtaining a vaccination, including working with large employers to bring vaccines to where people are.
[1] Merkley, E. and Loewen, P.J. (2021). Anti-intellectualism and the mass public’s response to the COVID-19 pandemic. Nature Human Behaviour, p. 1-10.
[2] For each variable, we present an estimate of how a one standard deviation change in the variable affects the probability of being vaccine willing. The lines through each symbol indicate the 95% confidence interval of the effect. Estimates to the left of the dashed line suggest that the factor reduces vaccine willingness, while those to the right suggest that it increases vaccine willingness.